Abstract

INTRODUCTION
Autologous stem cell transplantation (ASCT) is a relevant clinical option to consolidate some adult patients(pts) with acute myelogenous leukemia (AML) of the good and intermediate risk category in first complete remission (Bone Marrow Transplant. 2015;50:1495). It is still proposed in the 2017 ELN guidelines as consolidation for intermediate-risk genetics AML (Blood. 2017;129:424). Furthermore, the overal role of ASCT and the optimal conditioning pre ASCT for AML may need to be revisited due to the recent developments in the field including effective techniques for minimal residual disease (MRD) monitoring, new drug formulations and others. We have shown previously over the period from January 2005 to december 2015 (Cancer 2017 123:824), better outcomes following the combination of Busulfan and melphalan (BUMEL): in 225 pts who received BUMEL and 724 BUCY within 6 months after diagnosis, BUMEL compared to BUCY was associated with lower RI (34% versus 51%) higher LFS (62% versus 46%) and better OS (79% versus 65% ).In an effort to better study prognostic factors, we designed a larger study including all pts autografted from January 2000 to December 2016 with available cytogenetics. Since the availability of Melphalan remains an issue in some countries, we also wished to investigate whether some subgroups might specifically get benefit from BUMEL.
METHODS
Patients: All patients with available cytogenetics, autografted in the study period, in first complete remission, following either BUMEL or BUCY, were included. Busulfan was administered p.o. at the dose of 16 mg/kg or intravenously at the dose of 9.6 or 12.8mg/kg. Melphalan was given at the dose of 120 or 140 mg/m2. 1137 pts received BUCY and 512 BUMEL. The median follow up was 43 months for BUCY and 59 months for BUMEL pts.
Statistics: Endpoints were relapse incidence (RI), non-relapse mortality (NRM), leukemia-free survival (LFS) and overall survival (OS). Variables considered were age, sex and Karnofsky score, Cytogenetics risk groups, year of transplant, time from diagnosis to transplant, source of stem cells, pretransplant conditioning. All factors differing between the 2 conditioning were introduced in multivariate analyses. All interactions between conditioning and other prognostic factors were tested.
RESULTS
Primary analysis in the overall population:
The distribution of the characteristics of patients receiving BUCY and BUMEL was even except for the duration of the interval from diagnosis to transplant which was longer in the BUMEL group (5.5 months versus 4.7 months, p< 10-4). Cytogenetics were similar in BUCY and BUMEL. 117 pts (10%) in the BUCY group and 27 (5%) in the BUMEL group were reported as FLT3-ITD positive. We found an interaction between conditioning and the poor risk group defined as poor cytogenetics and/or presence of the FLT3-ITD mutation.
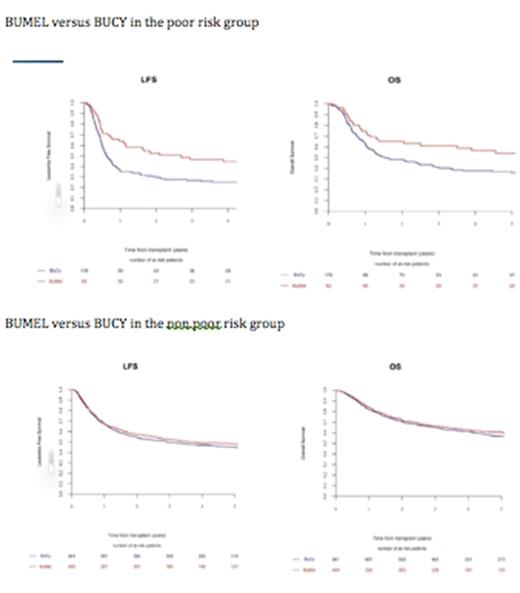
Separate analysis of the poor risk group (poor cytogenetics and/or FLT3-ITD mutation):176 patients received BUCY and 62 BUMEL. The distribution of the characteristics of patients receiving BUCY and BUMEL was even except for the duration of the interval from diagnosis to transplant. By multivariate analysis, BUMEL was associated with a lower RI (HR: 0.52 (0.34-0.78); p= 0.002), a better LFS (HR: 0.54 (0.36-0.80); p=0.002) and a better OS (HR: 0.61 (0.40-0.94); p=0.02). At five years, the RI post BUMEL versus BUCY was 53% versus 69%, the LFS 42% versus 25%, the OS 54% versus 36% (figure).
Separate analysis of the non poor risk group (good or intermediate cytogenetics, FLT3 wild type):
961 BUCY and 450 BUMEL patients belong to this group. At five years for BUCY and BUMEL respectively, the RI was 50% and 47%, the LFS 45% and 48% and the OS 56% and 60%, with no significant difference. By multivariate analysis, age, year of transplant and good versus intermediate cytogenetics were significant prognostic factors, but not the nature of the conditioning regimen.
CONCLUSION
In the current study, we demonstrated the superiority of BUMEL over BUCY in poor risk AML pts. It is conceivable that BUMEL is more cytoreductive than BUCY even in high risk pts more chemoresistant. This study and others confirms that ASCT may still be an option to consolidate patients with AML in CR1 at a time when maintenance post transplant including immune therapies may offer an alternative to allogeneic transplantation with a better quality of life in a carefully selected patient population.
Mohty: Sanofi: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal